热点推荐
热门图文
对于早期乳腺癌手术患者,如果切下来的腋窝淋巴结病理检查结果为阳性,那么区域淋巴结放疗已被大量随机对照研究证实可以降低局部区域复发、远处复发、乳腺癌所致死亡的风险。不过,如果术前化疗后腋窝淋巴结病理转阴,区域淋巴结放疗能否获益尚不明确。
2025年6月5日,国际四大医学期刊之一、创刊于1812年的美国麻省医学会《新英格兰医学杂志》正式发表全国乳腺肠道外科术后治疗研究基金会NSABP B-51研究暨肿瘤放疗学组RTOG 1304研究报告全文,对区域淋巴结放疗能否改善早期乳腺癌腋窝淋巴结活检阳性术前化疗后腋窝淋巴结病理转阴患者结局进行随机比较,该研究由美国国家卫生研究院下属国家癌症研究所资助。
NSABP B-51/RTOG 1304 (NCT01872975): Standard or Comprehensive Radiation Therapy in Treating Patients With Early-Stage Breast Cancer Previously Treated With Chemotherapy and Surgery
Official Title: A Randomized Phase III Clinical Trial Evaluating Post-Mastectomy Chestwall and Regional Nodal XRT and Post-Lumpectomy Regional Nodal XRT in Patients With Positive Axillary Nodes Before Neoadjuvant Chemotherapy Who Convert to Pathologically Negative Axillary Nodes After Neoadjuvant Chemotherapy
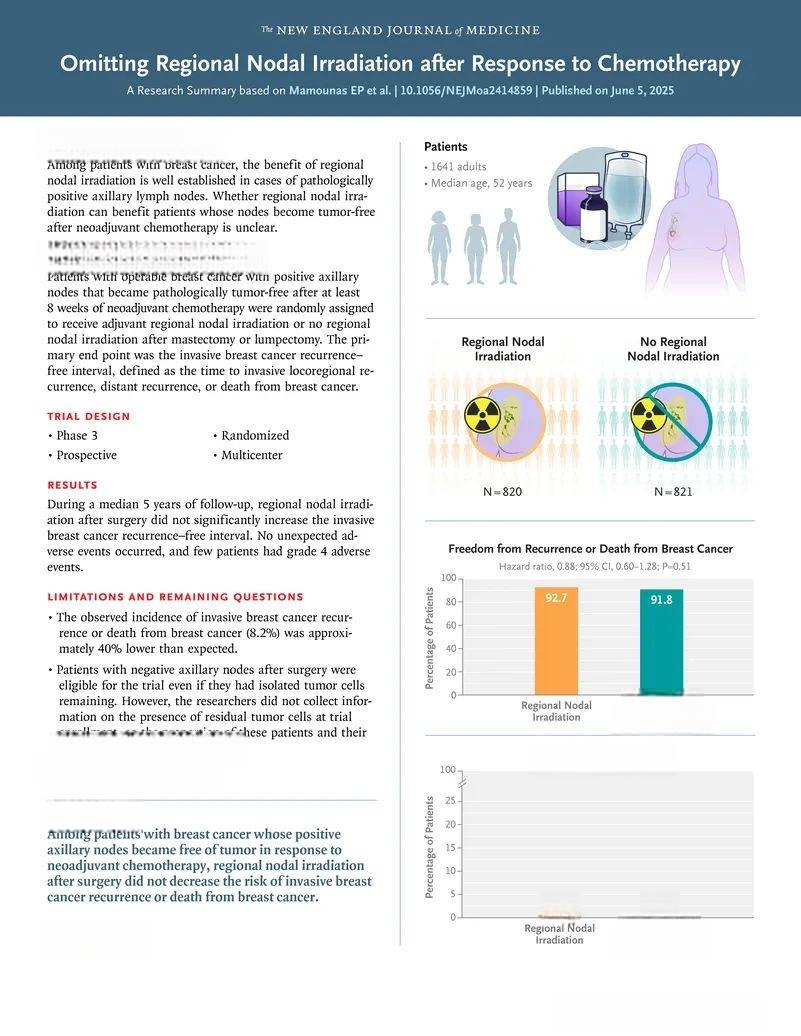
该国际多中心随机对照三期临床研究于2013年8月至2020年12月从美国、澳大利亚、加拿大、爱尔兰、以色列、日本、韩国入组术前临床分期为T1至T3(肿瘤最大直径:T1≤2厘米,T2>2厘米但≤5厘米,T3>5厘米)N1(术前活检证实1至3枚腋窝淋巴结阳性)M0(未远处转移)乳腺癌术前化疗后腋窝淋巴结病理转阴患者1641例,按1比1随机分为两组:其中820例给予区域淋巴结放疗、其余821例免予区域淋巴结放疗。主要终点为无乳腺浸润癌复发或乳腺癌所致死亡的间隔(无乳腺浸润癌复发间隔),次要终点包括无局部区域复发间隔、无远处复发间隔、无癌生存率和总生存率,并对安全性进行评定。
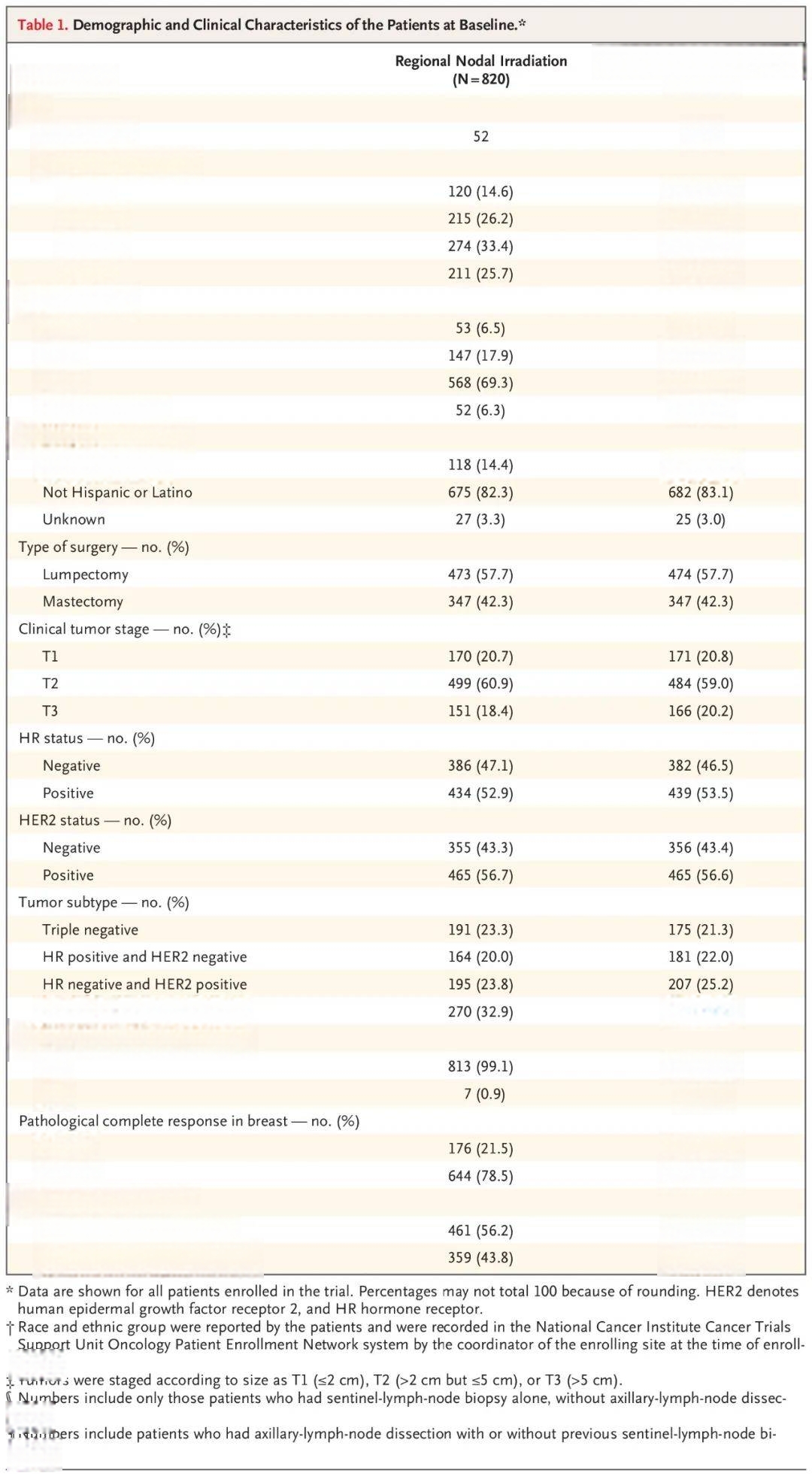
结果,截至2023年9月14日,获得1602例患者随访数据,其中46例(放疗组28例,免放疗组18例)缺少术前临床评定数据,故对其余1556例患者(放疗组772例,免放疗组784例)进行最终分析。
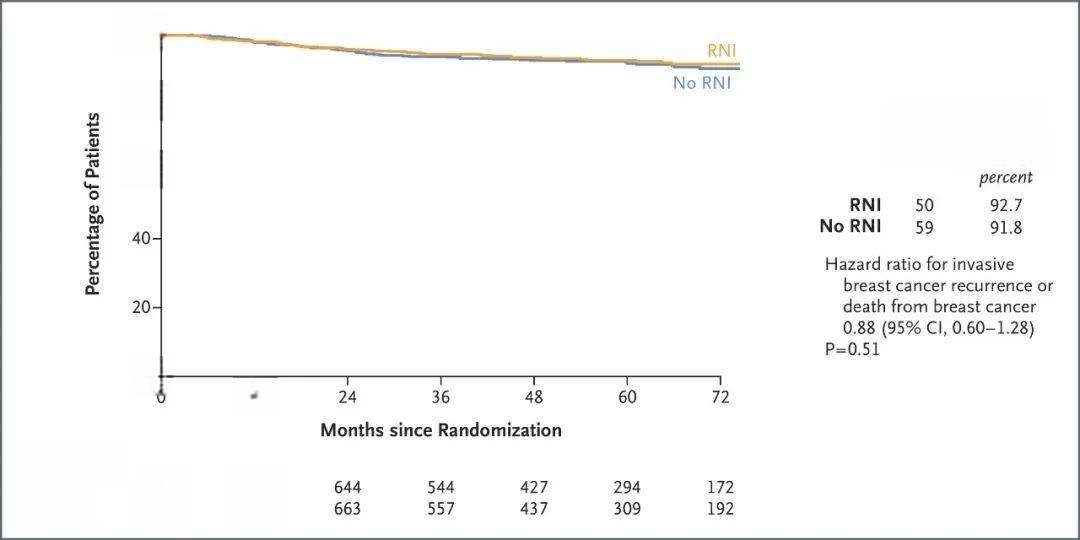
中位随访59.5个月,共发生109例主要终点事件(放疗组50例,免放疗组59例)。放疗组与未放疗组相比:
无乳腺浸润癌复发间隔相似(风险比:0.88,95%置信区间,0.60~1.28,P=0.51)
5年无乳腺浸润癌复发生存率相似(92.7%比91.8%)
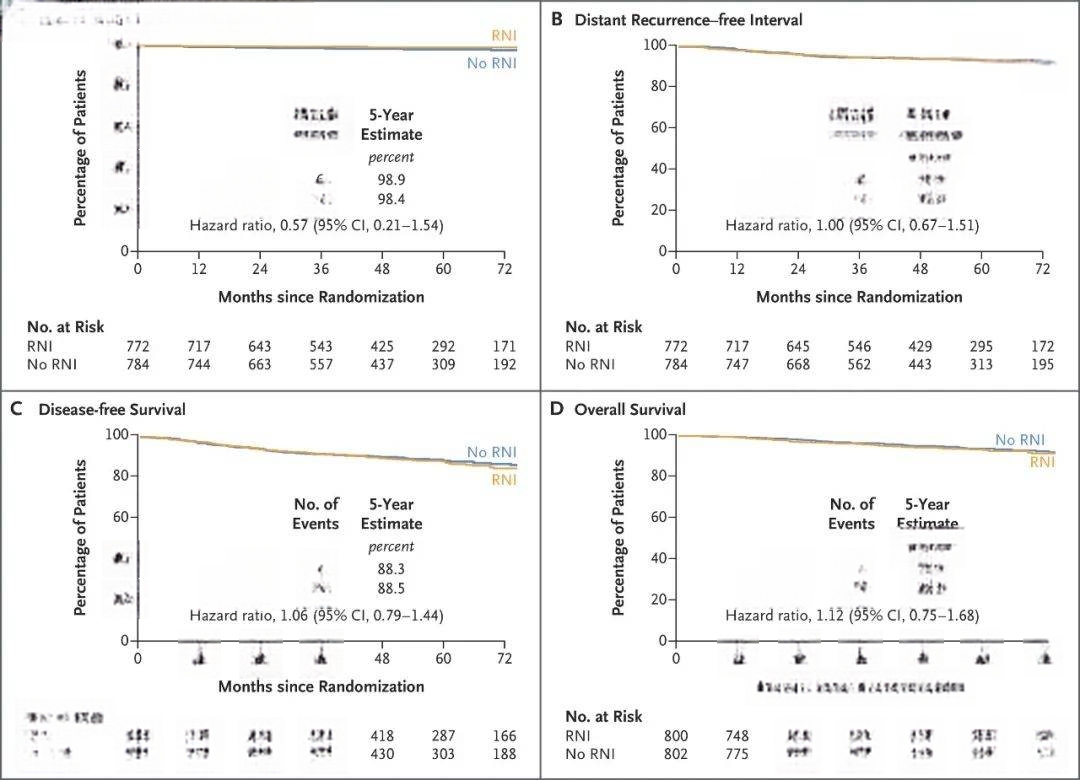
无局部区域复发间隔相似(风险比:0.57,95%置信区间:0.21~1.54)
无远处复发间隔相似(风险比:1.00,95%置信区间:0.67~1.51)
5年无癌生存率相似(88.3%比88.5%,风险比:1.06,95%置信区间:0.79~1.44)
5年总生存率相似(93.6%比94.0%,风险比,1.12,95%置信区间:0.75~1.68)

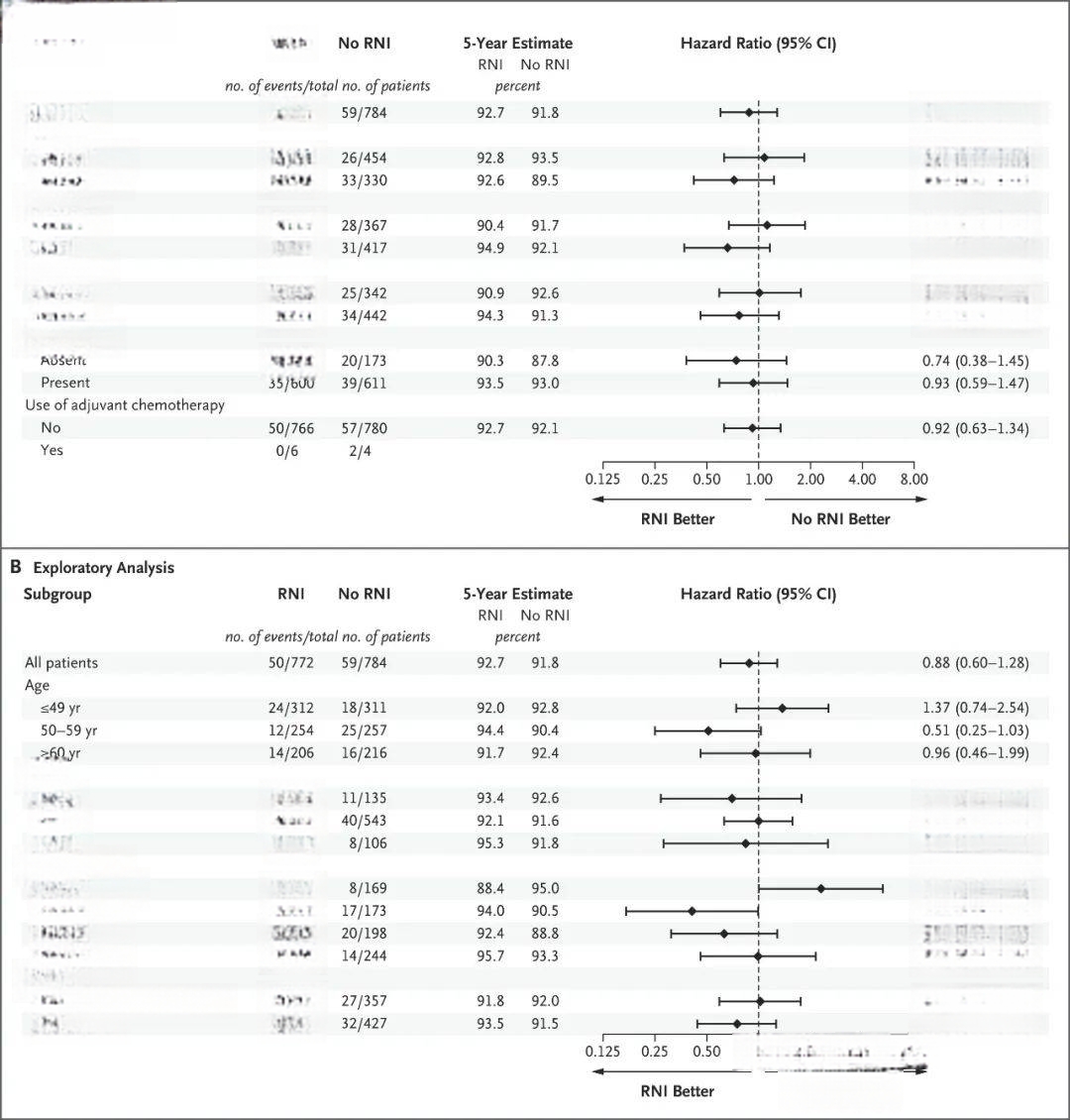
对主要终点进行亚组分析,结果发现放疗组与未放疗组相比,三阴性乳腺癌患者最有可能获益,激素受体阳性HER2阴性乳腺癌患者最不可能获益。
未报告方案定义治疗相关死亡病例,亦未见意外不良事件。放疗组与免放疗组相比,4级不良事件比例为0.5%比0.1%。
因此,该研究结果表明,对于术前化疗后腋窝淋巴结病理转阴患者,区域淋巴结放疗并未降低乳腺浸润癌复发或乳腺癌所致死亡风险。
N Engl J Med. 2025 Jun 5;392(21):2113-2124. IF: 96.2
Omitting Regional Nodal Irradiation after Response to Neoadjuvant Chemotherapy.
Mamounas EP, Bandos H, White JR, Julian TB, Khan AJ, Shaitelman SF, Torres MA, Vicini FA, Ganz PA, McCloskey SA, Lucas PC, Gupta N, Li XA, McCormick B, Smith B, Tendulkar RD, Kavadi VS, Matsumoto K, Seaward SA, Irvin WJ Jr, Lin JY, Mutter RW, Muanza TM, Stromberg J, Jagsi R, Weiss AC, Curran WJ Jr, Wolmark N.
AdventHealth Cancer Institute, Orlando, FL; NRG Oncology Statistical and Data Management Center, Pittsburgh; University of Pittsburgh School of Public Health, Pittsburgh; Allegheny Health Network Cancer Institute, Pittsburgh; National Surgical Adjuvant Breast and Bowel Project Pathology Lab, Pittsburgh; University of Pittsburgh Medical Center Hillman Cancer Center, Pittsburgh; University of Pittsburgh School of Medicine, Pittsburgh; National Surgical Adjuvant Breast and Bowel Project Foundation, Pittsburgh; University of Kansas Medical Center Comprehensive Cancer Center, Kansas City; Memorial Sloan Kettering Cancer Center, New York; University of Texas M.D. Anderson Cancer Center, Houston; Winship Cancer Institute, Emory University School of Medicine, Atlanta; Piedmont Oncology Institute, Atlanta; Michigan Healthcare Professionals, Pontiac; Jonsson Comprehensive Cancer Center, University of California, Los Angeles, Los Angeles; UCLA Fielding School of Public Health, Los Angeles; University of California, Los Angeles, Los Angeles; Mayo Clinic, Rochester, MN; Ohio State University, James Cancer Hospital, Columbus; Medical College of Wisconsin, Milwaukee; Case Western Reserve University Case Comprehensive Cancer Center, Cleveland; Taussig Cancer Center, Cleveland Clinic, Cleveland; Texas Oncology, US Oncology Network, The Woodlands; Kaiser Permanente National Cancer Institute Community Oncology Research Program, Vallejo, CA; Bon Secours Cancer Institute, Southeast Clinical Oncology Research Consortium, National Cancer Institute Community Oncology Research Program, Midlothian, VA; McGill University, Lady Davis Institute for Medical Research, Sir Mortimer B. Davis Jewish General Hospital, Montreal; Corewell Health, Oakland University Beaumont School of Medicine, Sterling Heights, MI; University of Rochester School of Medicine and Dentistry, Rochester, NY; Hyogo Cancer Center, Akashi, Hyogo, Japan.
BACKGROUND: The benefit of regional nodal irradiation in the treatment of breast cancer is well established for patients with pathologically positive axillary nodes, but whether it is also beneficial for patients whose nodes become pathologically tumor free (ypN0) after neoadjuvant chemotherapy remains unclear.
